Connect With Us
Blog

Ankle Disorders in the Elderly

As people age, the risk of developing ankle disorders rises, often due to decreased muscle strength, reduced balance, and the wear and tear on the joints over time. Seniors commonly face issues like arthritis, tendonitis, and ankle sprains, all of which can impact mobility and quality of life. Osteoarthritis is one of the most prevalent conditions among older adults, where the cartilage in the ankle joint wears down, leading to pain, stiffness, and limited movement. Rheumatoid arthritis, an autoimmune condition, can also inflame the ankle joints, causing discomfort and swelling. Tendonitis, especially in the Achilles tendon, is another concern. It often results from overuse or sudden increases in activity and causes swelling and pain. Ankle sprains, although common in all age groups, are particularly risky for seniors. Weakened ligaments and balance issues increase the chances of falling and injuring an ankle. Wearing supportive footwear and regular exercise can help maintain ankle strength and flexibility, reducing these risks. If you are a senior and have ankle pain, it is suggested that you schedule an appointment with a podiatrist for a proper diagnosis and appropriate treatment.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with David Williams, DPM from El Paso Feet. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Pain
Pain experienced in the ankle can be caused by a multitude of conditions. While the most common cause is an ankle sprain, other possible problems can include arthritis, gout, ankle instability, an ankle fracture, nerve compression, or tendinitis. In more serious cases, ankle pain can be a sign of improper alignment of the foot or an infection.
Ankle pain can often be accompanied by symptoms such as redness, swelling, stiffness, and warmth in the affected area. Pain can be described differently depending on the condition: short, stabbing pain and a dull ache are some examples. If such symptoms are persistent and do not improve after time, be sure to schedule an appointment with your local podiatrist.
Depending on the condition causing your ankle pain, different treatments may be prescribed by your podiatrist. For ankle sprains, the first step in treatment involves rest, ice, elevation, and compression. Be sure to avoid placing pressure on the ankle, use an ice pack several times a day, and use a compression bandage and elevation to reduce swelling. Other, more serious conditions may require the assistance of certain drugs and medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, or even cortisone injections.
Depending on the severity of your ankle pain and the condition behind it, recovery from ankle pain may take some time.
Consult with your foot and ankle doctor to best determine the cause of your ankle pain and the appropriate treatment.
Risk Factors and Symptoms of Tarsal Tunnel Syndrome

Tarsal tunnel syndrome, also known as posterior tibial neuralgia, is caused by compression of the posterior tibial nerve as it travels through the tarsal tunnel along the inside of the ankle. This compression can lead to pain, tingling, numbness, or a burning sensation in the foot and ankle. Risk factors for developing tarsal tunnel syndrome include having flat feet, which can stretch the nerve, previous ankle injuries that cause swelling, or conditions like arthritis and diabetes that lead to nerve damage or inflammation. Symptoms may worsen with prolonged standing, walking, or physical activity and pain can radiate into the toes or heel. If you have pain in this part of your foot, it is suggested that you visit a podiatrist for an accurate diagnosis and treatment.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact David Williams, DPM of El Paso Feet. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pain.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.
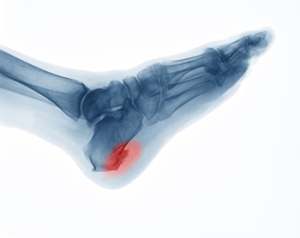
Risk Factors for Heel Spurs
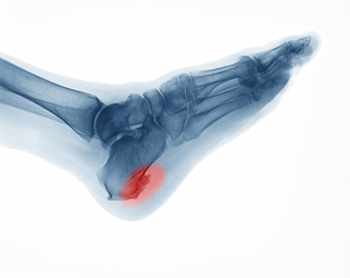
Heel spurs are calcium deposits that build up on the heel bone, often from repetitive strain on the foot’s ligaments and tendons. Several risk factors can increase the likelihood of developing a heel spur. High-impact activities like running, jumping, or dancing may put repeated stress on the heel. Long hours of standing on a hard surface can also contribute. Excess body weight places added pressure on the foot structures and may lead to small tears in the tissue, which may calcify into a spur. Foot structure plays a role as well, as people with flat feet or very high arches may be more prone to heel spurs. Wearing poorly fitting footwear, especially those with minimal arch or heel support, can worsen symptoms. A podiatrist may confirm the diagnosis of heel spurs through an X-ray or MRI scan, and may recommend cortisone injections, a walking boot, or surgery, if symptoms are long-lasting. If you have heel pain, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and appropriate treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact David Williams, DPM from El Paso Feet. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in El Paso, TX . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Stop Stubborn Plantar Warts with Swift

Are you frustrated by plantar warts? Plantar warts are commonly found on the soles of the feet or other areas that bear weight. They form due to exposure to the human papillomavirus (HPV). Effectively treat plantar warts with Swift, an FDA-cleared technology that has proven to be highly effective in the removal of plantar warts.
What Are the Symptoms of a Broken Pinky Toe?

A broken pinky toe often occurs from direct trauma, such as stubbing the toe against furniture or dropping a heavy object on the foot. It can also result from repetitive stress or overuse during physical activities that place pressure on the feet. Individuals with weakened bones or poor footwear support may be more susceptible. Symptoms of a broken pinky toe include sharp or throbbing pain, swelling, and visible bruising. The toe may appear crooked or misaligned, and walking can become difficult due to discomfort or instability. In some cases, the pain may persist even at rest. If you have broken your pinky toe, it is suggested that you promptly contact a podiatrist who can offer you appropriate treatment solutions.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact David Williams, DPM from El Paso Feet. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
Why Landing on Your Feet is Not Always Safe

Instinct tells us to land on our feet during a fall, but that does not always mean it is safe. The force of impact can send shockwaves through the feet, ankles, and legs, leading to serious injuries like fractures, sprains, and even long-term joint damage. Heel fractures, known as calcaneal fractures, are particularly common when landing from a height. The intense pressure can also damage the metatarsals or overstretch the Achilles tendon. Even if bones remain intact, the sudden impact can cause soft tissue injuries that lead to chronic pain or instability. Proper footwear, balance training, and strengthening exercises can help reduce fall risks. If you do fall, rolling or distributing impact across the body can lessen injury severity. When in doubt, it is suggested you get checked by a podiatrist, as what seems like a minor ache can turn into a long-term mobility issue.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with David Williams, DPM from El Paso Feet. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in El Paso, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.